The last menstrual period (LMP) is a term that holds significant importance in women’s health. It refers to the first day of a woman’s most recent menstrual bleeding. Understanding the concept of LMP is essential for monitoring reproductive health, planning pregnancies, and diagnosing various medical conditions. In this comprehensive article, we will explore what the last menstrual period means, its importance, how to track it, and its implications for health and fertility.
What is the Last Menstrual Period?
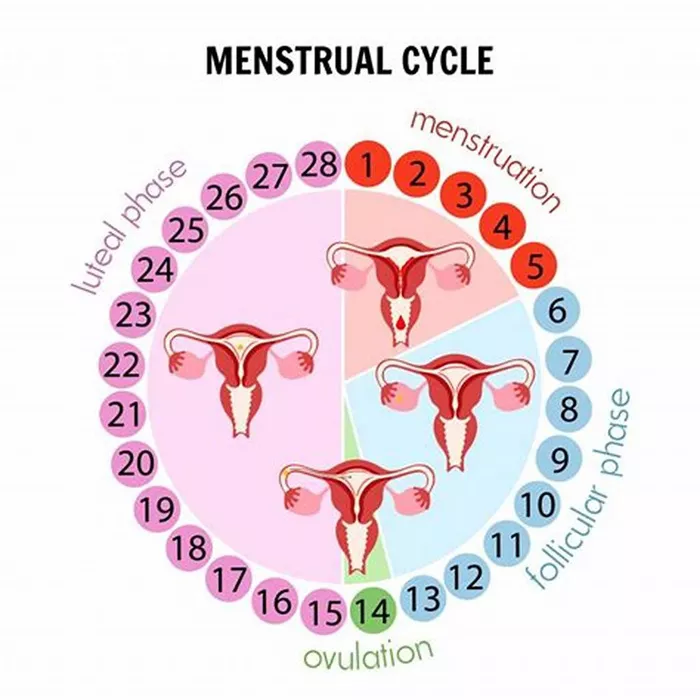
The last menstrual period (LMP) is the first day of a woman’s last menstrual bleeding before the onset of the next menstrual cycle. The menstrual cycle is a regular, natural process that prepares the female body for pregnancy. It typically lasts about 28 days, although cycles ranging from 21 to 35 days are considered normal. The menstrual cycle can be divided into several phases, including the menstrual phase, the follicular phase, ovulation, and the luteal phase.
The Menstrual Phase
The menstrual phase marks the beginning of the menstrual cycle. It is characterized by the shedding of the uterine lining, resulting in menstrual bleeding. This phase lasts for about 3 to 7 days and signals the start of a new cycle.
The Follicular Phase
Following the menstrual phase, the follicular phase begins. During this phase, the pituitary gland releases follicle-stimulating hormone (FSH), which stimulates the growth of ovarian follicles. Each follicle contains an egg, and as they mature, they produce estrogen. The follicular phase lasts from the end of menstruation until ovulation, typically around day 14 of a 28-day cycle.
Ovulation
Ovulation is the release of a mature egg from one of the ovarian follicles. This process is triggered by a surge in luteinizing hormone (LH) and usually occurs around the middle of the menstrual cycle, approximately 14 days before the start of the next period. Ovulation is a crucial phase for conception, as the egg is available for fertilization for about 12 to 24 hours.
The Luteal Phase
The luteal phase follows ovulation and lasts until the beginning of the next menstrual period. During this phase, the ruptured follicle transforms into the corpus luteum, which produces progesterone to prepare the uterine lining for a potential pregnancy. If fertilization does not occur, the corpus luteum breaks down, leading to a decrease in progesterone levels and the onset of menstruation.
Why is the Last Menstrual Period Important?
Tracking the last menstrual period is important for several reasons, including:
Predicting Ovulation and Fertile Window: Knowing the LMP helps women estimate their ovulation date and identify their most fertile days. This information is crucial for those trying to conceive or avoid pregnancy.
Estimating Due Date: In pregnancy, the LMP is used to estimate the due date. Healthcare providers calculate the gestational age of the pregnancy from the first day of the LMP, typically adding 280 days (40 weeks) to determine the expected date of delivery.
Monitoring Menstrual Health: Regular menstrual cycles are an indicator of overall reproductive health. Irregularities in the menstrual cycle can signal underlying health issues that may require medical attention.
Diagnosing Medical Conditions: Information about the LMP can aid in diagnosing various medical conditions, such as polycystic ovary syndrome (PCOS), thyroid disorders, and other hormonal imbalances.
Guiding Medical Procedures: The LMP is used to time certain medical procedures and treatments, such as fertility treatments, hormone therapy, and diagnostic tests.
How to Track the Last Menstrual Period
Tracking the LMP is relatively simple and can be done using various methods, including:
1. Menstrual Calendars
One of the most traditional methods of tracking the LMP is using a menstrual calendar. Women can mark the first day of their period on a calendar and continue to do so each month. This method helps visualize the menstrual cycle’s regularity and length over time.
2. Mobile Apps
In the digital age, many women prefer using mobile apps to track their menstrual cycles. These apps offer user-friendly interfaces and features such as reminders, cycle predictions, and symptom tracking. Popular menstrual tracking apps include Clue, Flo, and Period Tracker.
3. Basal Body Temperature (BBT) Charting
BBT charting involves measuring and recording body temperature every morning before getting out of bed. A slight increase in BBT occurs after ovulation due to the rise in progesterone. By tracking BBT, women can estimate their ovulation date and identify patterns in their menstrual cycle.
4. Cervical Mucus Monitoring
Observing changes in cervical mucus is another method to track the menstrual cycle. During the fertile window, cervical mucus becomes clear, stretchy, and resembles egg whites. This change indicates ovulation is approaching.
5. Ovulation Predictor Kits (OPKs)
OPKs detect the surge in LH that precedes ovulation. By using these kits, women can pinpoint their ovulation date and fertile window more accurately.
Factors Affecting the Menstrual Cycle
Several factors can influence the menstrual cycle’s regularity and length, including:
1. Age
Menstrual cycles can change with age. Adolescents may experience irregular cycles during the first few years after menarche (the first menstrual period). As women approach menopause, their cycles may become irregular again.
2. Stress
High levels of stress can disrupt the hormonal balance, leading to irregular menstrual cycles. Stress can affect the hypothalamus, the brain region that regulates the menstrual cycle.
3. Weight and Body Composition
Extreme weight loss or gain can impact the menstrual cycle. Low body weight, as seen in conditions like anorexia nervosa, can cause amenorrhea (absence of menstruation). Conversely, obesity can lead to irregular cycles and conditions like PCOS.
4. Physical Activity
Intense physical activity, especially in athletes, can affect the menstrual cycle. Low body fat and high levels of physical stress can lead to menstrual irregularities.
5. Hormonal Imbalances
Conditions such as PCOS, thyroid disorders, and hyperprolactinemia can cause hormonal imbalances that disrupt the menstrual cycle. These conditions require medical diagnosis and treatment.
6. Medications
Certain medications, including hormonal contraceptives, antipsychotics, and chemotherapy drugs, can affect the menstrual cycle. Women should discuss any concerns with their healthcare provider.
7. Underlying Health Conditions
Chronic illnesses, such as diabetes and autoimmune disorders, can impact menstrual health. Proper management of these conditions is essential for maintaining regular cycles.
The LMP and Pregnancy
The last menstrual period plays a crucial role in pregnancy planning and monitoring. Here’s how:
1. Calculating the Due Date
Healthcare providers use the LMP to estimate the due date. This method, known as Naegele’s rule, involves adding 280 days (40 weeks) to the first day of the LMP. While this calculation provides an approximate due date, it’s important to remember that only about 5% of babies are born on their estimated due date. Most births occur within two weeks before or after the due date.
2. Monitoring Pregnancy Progress
The LMP helps track the pregnancy’s progress and determine the baby’s gestational age. This information is vital for scheduling prenatal appointments, screenings, and ultrasounds.
3. Identifying Early Pregnancy Symptoms
Understanding the LMP can help women recognize early pregnancy symptoms, such as missed periods, nausea, and breast tenderness. These symptoms often prompt women to take a pregnancy test.
4. Managing Pregnancy Complications
In cases of complications such as ectopic pregnancy, miscarriage, or gestational diabetes, knowing the LMP can aid in diagnosis and treatment. Accurate dating of the pregnancy is crucial for appropriate medical management.
5. Postpartum Recovery
After childbirth, the LMP helps track postpartum recovery and the return of regular menstrual cycles. This information is important for family planning and monitoring overall health.
Common Misconceptions About the LMP
Despite its importance, several misconceptions surround the last menstrual period. Let’s address some of these myths:
1. Myth: The LMP is Always Accurate
While the LMP is a useful tool for estimating pregnancy dates, it may not always be accurate. Irregular cycles, incorrect recall of dates, and variations in ovulation timing can affect the accuracy. Ultrasound measurements in early pregnancy provide more precise dating.
2. Myth: Every Woman’s Cycle is 28 Days
The 28-day cycle is considered the average, but menstrual cycles can vary widely among women. Cycles ranging from 21 to 35 days are normal. Each woman’s cycle is unique and can fluctuate due to various factors.
3. Myth: You Can’t Get Pregnant During Your Period
While less likely, it is possible to conceive during menstruation. Sperm can survive in the female reproductive tract for up to five days. If ovulation occurs shortly after the period, pregnancy can result from intercourse during menstruation.
4. Myth: Stress Doesn’t Affect the Menstrual Cycle
Stress can significantly impact the menstrual cycle. High stress levels can disrupt hormonal balance, leading to irregular periods or missed cycles. Managing stress through relaxation techniques, exercise, and counseling can help maintain regular cycles.
5. Myth: Birth Control Doesn’t Affect the LMP
Hormonal contraceptives, such as birth control pills, patches, and intrauterine devices (IUDs), can alter the menstrual cycle. Some methods may cause lighter, shorter periods or eliminate them altogether. It’s important to understand how each contraceptive method affects menstruation.
The Role of Healthcare Providers
Healthcare providers play
a crucial role in helping women understand and manage their menstrual health, including the last menstrual period. Here are some ways healthcare providers can assist:
1. Menstrual Cycle Education
Healthcare providers can educate women about the menstrual cycle, including its phases, normal variations, and factors affecting cycle regularity. This knowledge empowers women to track their cycles effectively and recognize any abnormalities.
2. Fertility Awareness
For women trying to conceive, healthcare providers can offer guidance on fertility awareness methods, including tracking the LMP, monitoring basal body temperature, and observing cervical mucus changes. Understanding fertility patterns increases the chances of successful conception.
3. Menstrual Disorder Diagnosis and Treatment
Healthcare providers can evaluate and diagnose menstrual disorders such as irregular periods, heavy bleeding (menorrhagia), and absent periods (amenorrhea). Treatment options may include hormonal therapy, lifestyle modifications, or surgical interventions.
4. Pregnancy Counseling
During pregnancy planning or early pregnancy, healthcare providers offer counseling and prenatal care. They use information from the LMP and ultrasound dating to monitor fetal development, assess pregnancy risks, and provide appropriate care.
5. Contraceptive Guidance
For women seeking contraception, healthcare providers discuss available options, including hormonal contraceptives, barrier methods, and long-acting reversible contraceptives (LARCs). They explain how each method affects the menstrual cycle and helps women make informed choices.
6. Menopause Management
As women approach menopause, healthcare providers monitor changes in menstrual patterns, discuss symptoms such as hot flashes and mood changes, and offer management strategies, including hormone replacement therapy (HRT) and lifestyle adjustments.
7. Reproductive Health Screenings
Regular gynecological exams and screenings are essential for maintaining reproductive health. Healthcare providers perform pelvic exams, Pap smears, and screenings for sexually transmitted infections (STIs) to detect any abnormalities early and provide timely interventions.
Conclusion
The last menstrual period (LMP) serves as a cornerstone for understanding women’s reproductive health, fertility, and overall well-being. By tracking the LMP and monitoring menstrual cycles, women can gain valuable insights into their bodies, detect potential health issues, and make informed decisions about family planning and healthcare. Healthcare providers play a vital role in educating, supporting, and guiding women through various stages of their reproductive journey, ensuring optimal health outcomes and quality of life.