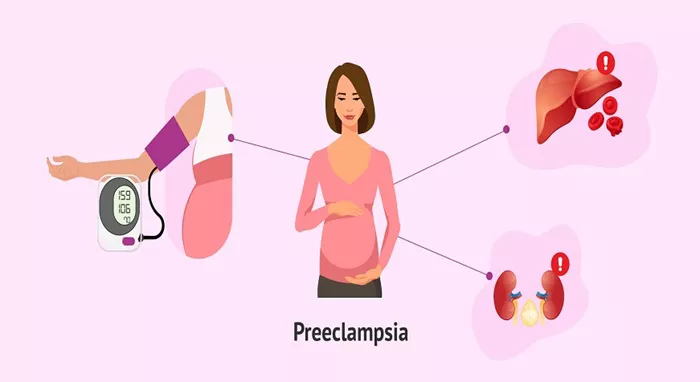
Preeclampsia is a serious medical condition that affects pregnant women, typically occurring after 20 weeks of gestation. Characterized by high blood pressure and often proteinuria (the presence of excess proteins in the urine), preeclampsia can lead to severe complications for both the mother and the baby if left untreated. Understanding the underlying causes of hypertension in preeclampsia is crucial for developing effective prevention and treatment strategies.
Overview of Preeclampsia and Hypertension
Preeclampsia is a complex disorder with multifactorial origins. The precise cause remains unclear, but several contributing factors have been identified. These include genetic predisposition, immune system abnormalities, vascular dysfunction, and improper placental development. Hypertension, or high blood pressure, is a hallmark of preeclampsia and serves as a key diagnostic criterion.
Hypertension in preeclampsia results from a combination of systemic vascular resistance and reduced blood flow to vital organs. This article delves into the mechanisms and factors contributing to the development of hypertension in preeclampsia.
Placental Dysfunction and Hypoxia
The placenta plays a central role in the pathogenesis of preeclampsia. In normal pregnancies, the placenta develops a network of blood vessels that facilitate the exchange of nutrients and oxygen between the mother and fetus. However, in preeclampsia, this process is disrupted.
Abnormal Trophoblast Invasion
Trophoblasts are specialized cells that form the outer layer of the placenta. They invade the maternal uterine lining to establish blood flow to the placenta. In preeclampsia, trophoblast invasion is shallow and incomplete. This results in poor remodeling of the spiral arteries, which are crucial for adequate blood supply to the placenta.
Placental Hypoxia
Due to inadequate trophoblast invasion, the placenta receives insufficient blood flow, leading to hypoxia (low oxygen levels). Hypoxic conditions within the placenta trigger the release of various factors that contribute to systemic endothelial dysfunction, a key player in the development of hypertension.
Endothelial Dysfunction
The endothelium is the inner lining of blood vessels and plays a vital role in regulating vascular tone and blood pressure. In preeclampsia, endothelial dysfunction is a prominent feature and contributes significantly to hypertension.
Imbalance of Vasodilators and Vasoconstrictors
Healthy endothelial function involves a delicate balance between vasodilators (substances that widen blood vessels) and vasoconstrictors (substances that narrow blood vessels). In preeclampsia, this balance is disrupted. There is a reduction in the production of vasodilators such as nitric oxide and prostacyclin, alongside an increase in vasoconstrictors like endothelin-1 and thromboxane. This imbalance results in increased vascular resistance and elevated blood pressure.
Oxidative Stress
Oxidative stress, characterized by an excess of reactive oxygen species (ROS), plays a critical role in endothelial dysfunction. In preeclampsia, placental hypoxia and other factors lead to increased ROS production. These reactive molecules damage endothelial cells, impairing their ability to regulate vascular tone effectively. The resulting endothelial dysfunction contributes to systemic hypertension.
Immune System Abnormalities
The immune system’s role in pregnancy is to facilitate tolerance to the fetus while protecting against infections. In preeclampsia, this delicate balance is disrupted, leading to immune system abnormalities that contribute to hypertension.
Inflammatory Response
Preeclampsia is associated with an exaggerated inflammatory response. Elevated levels of pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α) and interleukins are observed in affected women. These cytokines promote endothelial activation and dysfunction, contributing to increased vascular resistance and hypertension.
Autoantibodies
Some studies suggest that autoantibodies targeting specific receptors on endothelial cells may play a role in preeclampsia. For instance, autoantibodies against the angiotensin II type 1 receptor (AT1-AA) have been identified in preeclamptic women. These autoantibodies mimic the action of angiotensin II, a potent vasoconstrictor, leading to increased blood pressure.
Genetic Factors
Genetic predisposition is another important factor in the development of preeclampsia and its associated hypertension. Research has identified several genes that may contribute to the condition.
Genetic Variants
Certain genetic variants are associated with an increased risk of preeclampsia. These include genes involved in the regulation of blood pressure, endothelial function, and inflammatory responses. For example, polymorphisms in the angiotensinogen (AGT) gene and the methylenetetrahydrofolate reductase (MTHFR) gene have been linked to a higher risk of preeclampsia.
Family History
A family history of preeclampsia also increases the likelihood of developing the condition. This suggests that inherited genetic factors play a role in predisposing individuals to preeclampsia and its complications, including hypertension.
Angiogenic Imbalance
The balance between pro-angiogenic and anti-angiogenic factors is crucial for normal placental development and function. In preeclampsia, this balance is disrupted, contributing to hypertension.
Soluble Fms-like Tyrosine Kinase-1 (sFlt-1)
sFlt-1 is an anti-angiogenic factor that binds to and neutralizes pro-angiogenic factors such as vascular endothelial growth factor (VEGF) and placental growth factor (PlGF). In preeclampsia, levels of sFlt-1 are significantly elevated. The increased sFlt-1 sequesters VEGF and PlGF, impairing their ability to promote blood vessel formation and function. This leads to endothelial dysfunction and hypertension.
Decreased PlGF
PlGF is a pro-angiogenic factor essential for placental development. In preeclampsia, levels of PlGF are reduced, further contributing to the angiogenic imbalance. The decreased availability of PlGF exacerbates endothelial dysfunction and vascular resistance, resulting in hypertension.
Renin-Angiotensin-Aldosterone System (RAAS)
The RAAS is a hormonal system that regulates blood pressure and fluid balance. In preeclampsia, alterations in the RAAS contribute to hypertension.
Increased Angiotensin II Sensitivity
Angiotensin II is a potent vasoconstrictor that plays a critical role in regulating blood pressure. In preeclampsia, there is increased sensitivity to angiotensin II, leading to enhanced vasoconstriction and elevated blood pressure. This heightened sensitivity is partly due to the presence of AT1-AAs, which amplify the effects of angiotensin II.
Altered Aldosterone Levels
Aldosterone is a hormone that regulates sodium and water balance. In preeclampsia, aldosterone levels are often dysregulated. This can lead to increased sodium retention and blood volume expansion, contributing to hypertension.
Metabolic Factors
Metabolic abnormalities, including insulin resistance and obesity, are associated with an increased risk of preeclampsia and hypertension.
Insulin Resistance
Insulin resistance, a condition where the body’s cells become less responsive to insulin, is common in preeclampsia. Insulin resistance contributes to endothelial dysfunction and increased vascular resistance. Elevated insulin levels can also stimulate the production of vasoconstrictors, further exacerbating hypertension.
Obesity
Obesity is a well-known risk factor for preeclampsia. Excess body fat contributes to systemic inflammation, oxidative stress, and insulin resistance, all of which play a role in the development of hypertension. Adipose tissue, particularly visceral fat, secretes various pro-inflammatory cytokines and adipokines that promote endothelial dysfunction and vascular resistance.
Lifestyle and Environmental Factors
Lifestyle and environmental factors also influence the risk of developing preeclampsia and its associated hypertension.
Dietary Factors
Diet plays a significant role in blood pressure regulation. Diets high in salt, processed foods, and saturated fats can contribute to hypertension. Conversely, diets rich in fruits, vegetables, and whole grains are associated with a lower risk of hypertension.
Physical Activity
Regular physical activity is beneficial for maintaining healthy blood pressure levels. Sedentary lifestyles, on the other hand, are linked to an increased risk of hypertension and preeclampsia. Physical inactivity contributes to obesity, insulin resistance, and poor cardiovascular health, all of which are risk factors for preeclampsia.
Stress and Mental Health
Chronic stress and poor mental health can contribute to hypertension. Stress triggers the release of stress hormones such as cortisol and adrenaline, which can increase blood pressure. Additionally, stress and mental health issues can lead to unhealthy lifestyle behaviors, such as poor diet and lack of exercise, further increasing the risk of hypertension.
Clinical Implications and Management
Understanding the causes of hypertension in preeclampsia is essential for effective management and prevention. Several strategies can be employed to manage hypertension in preeclampsia and reduce the risk of complications.
Monitoring and Early Detection
Regular prenatal care is crucial for early detection and management of preeclampsia. Blood pressure monitoring and urine tests for proteinuria are standard practices during prenatal visits. Earrol blood pressure. Additionally, maintaining a healthy weight through diet and exercise is beneficial.
Medications
In some cases, medications are necessary to manage hypertension in preeclampsia. Several classes of antihypertensive drugs can be used, but the choice of medication must consider the safety of both the mother and the fetus.
Antihypertensive Medications
Methyldopa: This is a commonly used antihypertensive medication in pregnancy. It has a long history of safety and effectiveness in reducing blood pressure without significant adverse effects on the fetus.
Labetalol: A combined alpha and beta-blocker, labetalol is another frequently prescribed drug for managing hypertension in pregnant women. It is effective in reducing blood pressure and is generally well tolerated.
Nifedipine: This calcium channel blocker is used for its vasodilatory effects. It is particularly useful in managing acute hypertension in preeclampsia.
Hydralazine: Often used in severe cases of hypertension, hydralazine acts by relaxing vascular smooth muscles, thus lowering blood pressure.
Corticosteroids
In cases where preeclampsia occurs before 34 weeks of gestation, corticosteroids may be administered to enhance fetal lung maturity. This preparation is crucial if an early delivery becomes necessary due to severe preeclampsia or eclampsia.
Delivery
The definitive treatment for preeclampsia is delivery of the baby and placenta. The timing of delivery depends on the severity of the condition and the gestational age. In cases of severe preeclampsia, particularly when it occurs early in pregnancy, the risks to the mother may necessitate early delivery, even if it means delivering a preterm baby.
Research and Future Directions
Ongoing research continues to explore the underlying mechanisms of preeclampsia and the associated hypertension, aiming to develop more effective prevention and treatment strategies.
Biomarker Identification
Identifying reliable biomarkers for early detection of preeclampsia is a key area of research. Biomarkers such as sFlt-1, PlGF, and various genetic markers are under investigation. Early identification of women at risk for preeclampsia can lead to better monitoring and timely interventions.
Genetic Studies
Genetic research is uncovering the hereditary components of preeclampsia. Studies involving genome-wide association studies (GWAS) and family-based genetic analyses are identifying genes that contribute to the condition. Understanding these genetic factors could lead to personalized approaches to prevention and treatment.
Immunological Therapies
Given the immune system’s role in preeclampsia, immunological therapies are being explored. Treatments aimed at modulating the immune response, such as the use of immunoglobulins or immune-modulating drugs, hold potential for reducing the risk and severity of preeclampsia.
Nutritional Interventions
Research into nutritional interventions is ongoing. Studies are examining the impact of various nutrients, such as omega-3 fatty acids, antioxidants, and vitamins, on the prevention and management of preeclampsia. Dietary supplements and tailored nutrition plans may offer new avenues for reducing the risk of hypertension in preeclampsia.
Clinical Trials
Clinical trials are critical for testing new treatments and interventions for preeclampsia. These trials help establish the safety and efficacy of potential therapies, providing evidence-based options for managing the condition.
Conclusion
Hypertension in preeclampsia is a complex condition resulting from multiple interrelated factors, including placental dysfunction, endothelial dysfunction, immune system abnormalities, genetic predisposition, angiogenic imbalance, and metabolic and lifestyle factors. Understanding these mechanisms is crucial for developing effective prevention and treatment strategies.
Early detection and timely management of preeclampsia are essential to reduce the risk of severe complications for both the mother and the baby. Regular prenatal care, lifestyle modifications, and appropriate medical interventions play a key role in managing hypertension in preeclampsia.
Ongoing research continues to shed light on the underlying causes of preeclampsia, offering hope for better diagnostic tools and more effective treatments in the future. Through a combination of scientific advancements and comprehensive clinical care, the goal of reducing the incidence and impact of preeclampsia and its associated hypertension is within reach.