Fluid in the womb, also known as hydrometra, is a condition that can affect women of various ages. It refers to the presence of serous fluid within the uterine cavity. The causes of fluid accumulation in the womb are diverse, ranging from hormonal imbalances to structural abnormalities and infections. Understanding these causes is crucial for effective diagnosis and treatment. This article explores ten common causes of fluid in the womb, their implications, and potential management strategies.
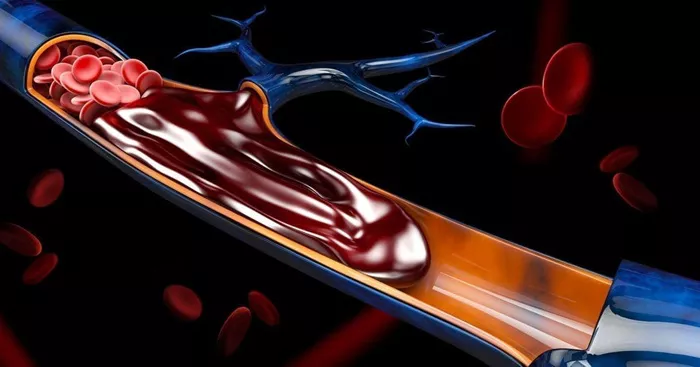
What is Fluid in the Womb?
Fluid in the womb, or hydrometra, involves the retention of clear, watery fluid in the uterus. This condition can sometimes be asymptomatic but may also present with various symptoms, such as pelvic pain, abnormal bleeding, or a feeling of fullness in the lower abdomen. Accurate diagnosis and understanding the underlying cause are essential for appropriate management and treatment.
1. Hormonal Imbalances
Hormonal imbalances are one of the primary causes of fluid accumulation in the womb.
Estrogen Dominance
Estrogen dominance occurs when there is an excess of estrogen relative to progesterone. This imbalance can cause the endometrial lining to thicken abnormally, leading to fluid retention. Estrogen dominance is often seen in conditions like polycystic ovary syndrome (PCOS) and during perimenopause.
Progesterone Deficiency
Progesterone is crucial for maintaining the uterine lining and regulating menstrual cycles. A deficiency in progesterone can disrupt normal endometrial shedding, leading to fluid accumulation. This imbalance can be due to various factors, including stress, poor diet, and certain medical conditions.
2. Cervical Stenosis
Cervical stenosis is the narrowing or closure of the cervical canal, which can obstruct the normal outflow of uterine secretions, resulting in fluid buildup.
Causes of Cervical Stenosis
Cervical stenosis can be congenital or acquired. Acquired causes include surgical procedures such as cone biopsy, radiation therapy for pelvic cancers, and severe infections like cervicitis.
Symptoms and Diagnosis
Symptoms of cervical stenosis include pelvic pain, abnormal uterine bleeding, and difficulty in menstruation. Diagnosis typically involves a pelvic examination and imaging studies like ultrasound or MRI.
3. Uterine Polyps and Fibroids
Benign growths such as polyps and fibroids can interfere with the normal drainage of uterine secretions, leading to fluid retention.
Uterine Polyps
Uterine polyps are small, benign growths that form on the inner wall of the uterus. They can obstruct the cervical canal, leading to fluid buildup.
Fibroids
Fibroids are non-cancerous tumors that grow in or around the uterus. Depending on their size and location, fibroids can block the normal outflow of fluids, contributing to hydrometra.
4. Pelvic Inflammatory Disease (PID)
Pelvic Inflammatory Disease (PID) is an infection of the female reproductive organs, often caused by sexually transmitted infections (STIs).
How PID Causes Hydrometra
PID can lead to scarring and obstruction of the fallopian tubes and uterine cavity, causing fluid retention. Chronic PID can result in significant structural damage, increasing the risk of hydrometra.
Symptoms and Treatment
Symptoms of PID include pelvic pain, fever, abnormal vaginal discharge, and painful intercourse. Treatment involves antibiotics to address the underlying infection and may require surgical intervention to remove any scar tissue.
5. Endometritis
Endometritis is the inflammation of the endometrium, the inner lining of the uterus, often caused by infections or certain medical procedures.
Causes of Endometritis
Endometritis can occur after childbirth, miscarriage, or procedures like dilation and curettage (D&C). It can also result from untreated pelvic infections.
Implications and Management
Endometritis can lead to fluid accumulation in the womb due to inflammation and obstruction. Treatment typically involves antibiotics to clear the infection and anti-inflammatory medications to reduce symptoms.
6. Congenital Anomalies
Congenital anomalies of the uterus can disrupt normal fluid drainage, leading to hydrometra.
Types of Congenital Anomalies
Bicornuate Uterus: A uterus with two cavities instead of one.
Septate Uterus: A uterus divided by a fibrous or muscular septum.
Didelphys Uterus: A condition where a woman has two separate uterine cavities and cervices.
Diagnosis and Treatment
Diagnosis of congenital anomalies often involves imaging studies like ultrasound, MRI, or hysterosalpingography. Treatment may include surgical correction to restore normal uterine anatomy.
7. Radiation Therapy
Radiation therapy, often used to treat cancers, can damage the uterine lining and lead to fluid retention.
Effects of Radiation on the Uterus
Radiation can cause scarring and fibrosis of the uterine tissues, leading to stenosis and obstructed fluid outflow. This condition is more common in women who have received radiation therapy for pelvic cancers.
Management
Management of radiation-induced hydrometra involves addressing the underlying scarring and may require surgical intervention to restore normal uterine drainage.
8. Medical Procedures
Certain medical procedures can result in fluid accumulation in the womb.
Dilation and Curettage (D&C)
D&C is a procedure used to diagnose and treat various uterine conditions. However, it can sometimes lead to scarring and fluid retention.
Hysteroscopy
Hysteroscopy involves inserting a camera into the uterine cavity to diagnose and treat conditions like polyps and fibroids. While generally safe, it can occasionally cause scarring or infections, leading to hydrometra.
9. Menopausal Changes
Menopausal changes can contribute to fluid accumulation in the womb due to hormonal fluctuations and changes in the uterine lining.
Postmenopausal Atrophy
After menopause, the endometrial lining can become thin and atrophic. This can lead to poor drainage of uterine secretions and fluid buildup.
Hormone Replacement Therapy (HRT)
Women on HRT, particularly those taking estrogen without progesterone, can develop endometrial hyperplasia, which may result in fluid retention.
10. Chronic Health Conditions
Certain chronic health conditions can predispose women to fluid accumulation in the womb.
Diabetes
Diabetes can affect blood flow and tissue healing, increasing the risk of infections and structural abnormalities that lead to hydrometra.
Autoimmune Disorders
Autoimmune disorders like lupus and rheumatoid arthritis can cause inflammation and scarring in the reproductive organs, contributing to fluid retention.
Conclusion
Fluid accumulation in the womb, or hydrometra, can result from various factors including hormonal imbalances, structural abnormalities, infections, and medical procedures. Understanding the underlying causes, recognizing symptoms, and seeking timely medical care are crucial for effective diagnosis and management.
By addressing hormonal imbalances, treating infections promptly, managing chronic health conditions, and maintaining good reproductive health practices, women can reduce the risk of fluid accumulation in the womb and associated complications.
Regular gynecological exams, safe sexual practices, and lifestyle modifications play key roles in preventing hydrometra and promoting overall reproductive well-being. Collaborative efforts between healthcare providers and individuals can lead to better outcomes and improved quality of life for women affected by fluid in the womb.