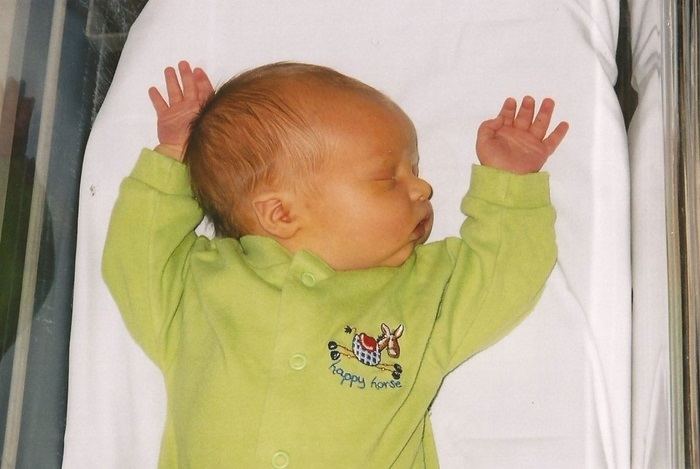
Neonatal jaundice is a common condition characterized by the yellowing of a newborn’s skin and eyes. This yellow discoloration is due to high levels of bilirubin, a yellow pigment produced during the normal breakdown of red blood cells. In neonates, the liver is often not mature enough to efficiently process and remove bilirubin from the bloodstream, leading to its accumulation.
Prevalence
Neonatal jaundice is extremely common, affecting about 60% of full-term infants and up to 80% of preterm infants within the first week of life. While it is usually a temporary and harmless condition, it requires careful monitoring to prevent complications.
Causes
There are two main types of neonatal jaundice: physiological and pathological.
1. Physiological Jaundice: This is the most common type and occurs in almost all newborns. It typically appears between the second and fourth days of life and resolves on its own within two weeks. Physiological jaundice is due to the immaturity of the baby’s liver, which is unable to process bilirubin as efficiently as in older children and adults.
2. Pathological Jaundice: This type of jaundice is less common but more serious. It usually appears within the first 24 hours of life and can be caused by various underlying health issues such as: Conditions like Rh incompatibility or ABO incompatibility where the mother’s antibodies attack the baby’s red blood cells.Sepsis or other infections that affect the liver’s ability to process bilirubin.
Symptoms
The primary symptom of neonatal jaundice is the yellowing of the skin and the whites of the eyes (sclera). This yellowing usually starts on the face and moves down to the chest, abdomen, and legs. Other symptoms to watch for include:
1. Poor feeding or sucking
2. Lethargy
3. Dark, yellow urine (in a newborn, urine should typically be colorless)
4. Pale-colored stool (normal stool should be yellow or orange)
Risk Factors
Certain factors increase the risk of developing jaundice in newborns, including:
1. Prematurity: Preterm babies have an even less developed liver function.
2. Bruising during birth: Excessive bruising can lead to higher bilirubin levels due to the breakdown of a larger number of red blood cells.
3. Breastfeeding: While breastfeeding is beneficial, poor feeding habits or issues with latching can lead to dehydration and decreased bilirubin excretion.
4. Ethnic Background: East Asian, Mediterranean, or Native American descent have higher incidences of neonatal jaundice.
5. Sibling History: A family history of neonatal jaundice increases the likelihood in subsequent children.
6. Blood Group Incompatibility: Rh or ABO blood type incompatibility between the mother and baby.
Diagnosis
Neonatal jaundice is diagnosed through a combination of physical examination and laboratory tests. Key steps include:
1. Visual Assessment: Observing the yellowing of the skin and eyes.
2. Transcutaneous Bilirubinometry: A non-invasive method that uses a device to estimate bilirubin levels through the skin.
3. Blood Tests: If jaundice is significant or appears within the first 24 hours, a blood test measuring total serum bilirubin (TSB) is performed. This helps determine the severity and guides treatment.
Treatment
Treatment depends on the severity of the jaundice and the underlying cause. Common treatments include:
1. Phototherapy: The most common treatment for significant jaundice. The baby is placed under special blue spectrum lights that help break down bilirubin in the skin.
2. Exchange Transfusion: In severe cases, the baby may need a blood transfusion to rapidly reduce bilirubin levels.
3. Intravenous Immunoglobulin (IVIg): Used in cases of Rh incompatibility, IVIg can reduce the levels of antibodies that attack the baby’s red blood cells.
4. Proper Feeding: Ensuring the baby is well-fed, either through breastfeeding or formula, helps reduce bilirubin levels by promoting bowel movements which excrete bilirubin.
Prevention and Monitoring
While not all cases of jaundice can be prevented, some strategies can reduce the risk and ensure early detection:
1. Frequent Feeding: Newborns should be fed at least 8 to 12 times a day in the first days of life to help pass bilirubin through the stool.
2. Early and Regular Monitoring: Healthcare providers should check bilirubin levels within the first 24 hours, especially if the baby is at high risk.
3. Education for Parents: Parents should be educated on how to recognize jaundice and the importance of follow-up appointments.
When to Contact a Healthcare Provider
Immediate medical attention is necessary if:
1. Jaundice appears within the first 24 hours of life.
2. The baby becomes increasingly yellow.
3. The baby has difficulty waking, feeding, or shows signs of illness.
4. The baby’s jaundice does not improve after two weeks or seems to worsen.
Parental Support
Dealing with neonatal jaundice can be stressful for parents. Resources and support groups can offer valuable information and emotional support. It’s important for parents to stay in touch with their healthcare providers, attend all follow-up appointments, and reach out with any concerns about their baby’s health.
In summary, neonatal jaundice is a common and usually manageable condition, but it requires vigilance and proper care to prevent complications. Comprehensive education for parents and caregivers is essential to ensure timely recognition and treatment of this condition. Always consult healthcare professionals for personalized medical advice to safeguard the health and well-being of the newborn.