Jaundice is a common condition in newborns that can often cause concern among parents. Characterized by the yellowing of the skin and eyes, jaundice occurs due to elevated levels of bilirubin in the blood. While it is a relatively common occurrence, understanding the threshold levels of bilirubin that indicate jaundice, its types, treatment options, and when to seek medical advice are crucial for parents and caregivers. This article aims to provide comprehensive information on jaundice in newborns, addressing the search intent behind “What Level Bilirubin Is Jaundice in Newborns” and offering actionable guidance for its management.
Definition of Jaundice
Jaundice, medically known as icterus, is a condition characterized by the yellow discoloration of the skin and eyes. It occurs when there is an excess buildup of bilirubin in the blood, a yellow pigment produced by the breakdown of red blood cells. Bilirubin is typically processed by the liver and excreted from the body through urine and stool. However, in newborns, the liver may take some time to mature and efficiently process bilirubin, leading to its accumulation in the blood and subsequent jaundice.
The visible yellowing of the skin and eyes is the most apparent symptom of jaundice. Other signs may include yellowing of the mucous membranes, such as the inside of the mouth, poor feeding, lethargy, and dark urine. Jaundice usually appears within the first few days of life and may resolve on its own as the baby’s liver matures and becomes more efficient at processing bilirubin.
Bilirubin Levels
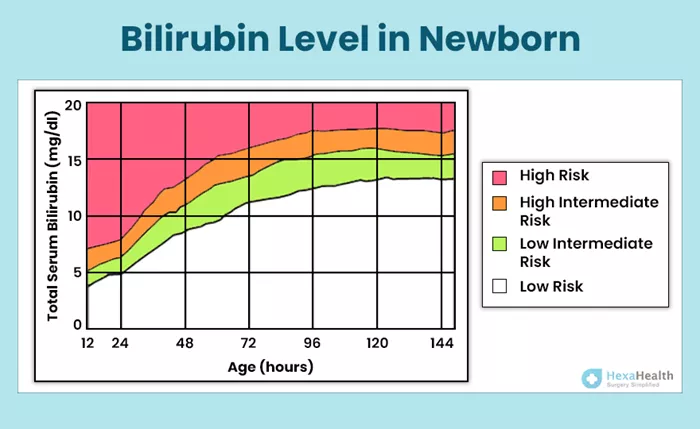
Understanding the bilirubin level thresholds is crucial in identifying when jaundice is present in newborns. Bilirubin levels are typically measured in milligrams per deciliter (mg/dL) of blood. Jaundice becomes visible on the sclera (the white part of the eyes) at a bilirubin level of approximately 2 to 3 mg/dL. Yellowing of the face typically occurs at levels of around 4 to 5 mg/dL.
It’s important to note that while these thresholds provide a general guideline, the severity of jaundice and the associated risks can vary based on factors such as the baby’s gestational age, overall health, and any underlying conditions.
Types of Jaundice
There are different types of jaundice that newborns may experience:
1. Physiological Jaundice: This is the most common type of jaundice in newborns and occurs as a normal response to the breakdown of red blood cells and the immaturity of the liver. It typically appears within the first few days of life and resolves on its own as the baby’s liver matures.
2. Breastfeeding Jaundice: Breastfeeding jaundice may occur when there is inadequate milk intake, leading to dehydration and reduced elimination of bilirubin. It can often be addressed by ensuring proper breastfeeding techniques and frequent feeding sessions.
3. Breast Milk Jaundice: Breast milk jaundice is less common and occurs when certain components in breast milk interfere with the liver’s ability to process bilirubin. It may persist for several weeks but usually resolves without treatment.
Treatment Options
Treatment for jaundice in newborns depends on the severity of the condition and the underlying cause. In many cases, mild jaundice may not require treatment and may resolve on its own as the baby’s liver matures. However, if bilirubin levels are high or rising rapidly, medical intervention may be necessary.
Phototherapy is a common treatment for jaundice in newborns. During phototherapy, the baby is placed under special lights that help break down bilirubin in the skin. In more severe cases, exchange transfusion may be required to replace the baby’s blood with fresh donor blood.
When to Seek Medical Advice
While jaundice is common in newborns, high bilirubin levels can pose risks if left untreated. It’s essential for parents to monitor their baby for signs of jaundice and seek medical advice if they notice persistent yellowing of the skin and eyes, poor feeding, or lethargy.
Untreated jaundice can lead to complications such as kernicterus, a rare but serious condition characterized by the accumulation of bilirubin in the brain. Kernicterus can cause permanent brain damage and neurological impairments.
Prevention and Monitoring
Preventing severe jaundice involves ensuring adequate feeding and monitoring bilirubin levels, especially in the first week of life. Breastfeeding should be initiated within the first hour after birth, and frequent feeding sessions should be encouraged to promote bilirubin elimination. Healthcare providers may recommend bilirubin testing for high-risk infants or those exhibiting signs of jaundice.
Parents can monitor their baby’s jaundice by observing changes in skin color and noting any feeding difficulties or changes in behavior. Regular check-ups with healthcare providers can help ensure that jaundice is promptly identified and managed.
Parental Support
Experiencing jaundice in a newborn can be worrying for parents, but it’s essential to remember that it is a common and usually temporary condition. Providing reassurance to parents about the manageability of jaundice and offering support can help alleviate concerns.
Encouraging parents to communicate openly with healthcare providers, ask questions, and seek support from family and friends can help them navigate this challenging time. Additionally, promoting bonding and skin-to-skin contact between parents and their baby can aid in their overall well-being.
In conclusion, jaundice is a common occurrence in newborns, typically caused by elevated bilirubin levels in the blood. Understanding the threshold levels of bilirubin that indicate jaundice, its types, treatment options, and when to seek medical advice is essential for parents and caregivers. By following preventative measures, monitoring bilirubin levels, and seeking timely medical advice when needed, parents can effectively manage jaundice in newborns and ensure the health and well-being of their baby.